Guidelines for People with Diabetes
If you take insulin to control your blood sugar, ask your physician what amount of your medication you should take the day of the test. Often, your physician will tell you to take only half of your usual morning dose and to eat a light meal four hours before the test.
If you take pills to control your blood sugar, do not take your medication until after the test is complete.
Do not take your diabetes medication and skip a meal before the test.
If you own a glucose monitor, bring it with you to check your blood sugar levels before and after your test. If you think your blood sugar is low, tell the lab personnel immediately. Plan to eat and take your diabetes medication following your test.
What should I wear on the day of the test?
Please wear or bring comfortable clothes and shoes suitable for walking. Please do not bring valuables. You will be given a locker to store your belongings during the test.
What happens during the test?
Your test will take place in the Echo Lab. The testing area is supervised by a physician.
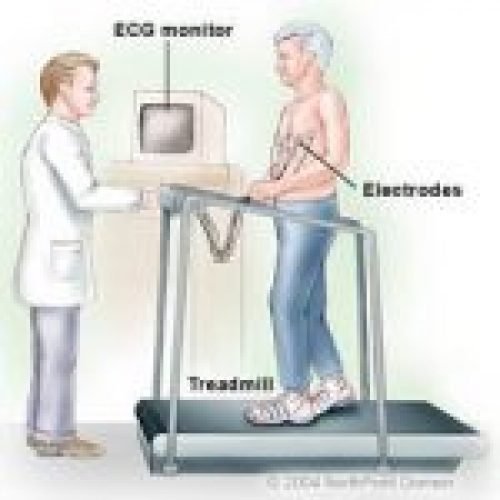
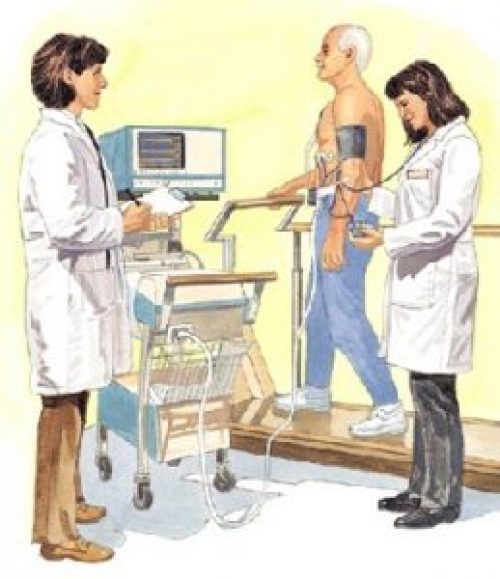
First, a cardiac sonographer will gently rub 10 small areas on your chest and place electrodes (small, flat, sticky patches) on these areas. The electrodes are attached to an electrocardiograph (EKG) monitor that charts your heart’s electrical activity during the test.
Before you start exercising, the sonographer will perform a resting EKG, measure your resting heart rate and take your blood pressure.
The sonographer will ask you to lie on your left side on an exam table so he or she can perform a resting echocardiogram (also called an “echo”). An echocardiogram is a graphic outline of the heart’s movement created from ultrasound vibrations echoed from the heart’s structures. The sonographer will place a wand (called a transducer) on your chest to view an outline of the heart’s movement.
After the echo test, you will exercise on a treadmill or stationary cycle. The lab personnel will ask you to start exercising and will gradually increase the intensity of exercise. You will be asked to continue exercising until you are exhausted.
At regular intervals, the lab personnel will ask how you are feeling. Please tell them if you feel chest, arm or jaw pain or discomfort; short of breath, dizzy, lightheaded or if you have any other unusual symptoms.
The lab personnel will watch for any changes on the EKG monitor that suggest the test should be stopped.
When you cannot exercise any longer, you will get off the treadmill,* quickly return to the exam table and lie on your left side so the sonographer can perform another echocardiogram.
*If you were exercising on a bike, the sonographer may perform the echo test while you are still pedaling. You may be asked to quickly return to the exam table for another echocardiogram after exercising.
After the test, you will walk slowly for a few minutes to cool down. Your heart rate, blood pressure and EKG will continue to be monitored until the levels are returning to normal.
How will I feel during the test?
You will be encouraged to exercise until you are exhausted. It is normal for your heart rate, blood pressure, breathing rate and perspiration to increase.
As you stop exercising suddenly, it is normal to feel a little unsteady when getting off the treadmill and onto the exam table for the echocardiogram.
How long does the test take?
The appointment will take about 60 minutes. The actual exercise time is usually between seven and 12 minutes.
How do I get the results of my test?
After a cardiologist has reviewed your test, the results will be entered into your electronic medical record. Your physician will have access to the results and will discuss them with you.
The exercise stress echo test involves exercising on a treadmill or stationary cycle while you are closely monitored.
Why is this test performed?
The test is used to:
Determine how well your heart tolerates activity
Evaluate the function of your heart and valves
Determine your likelihood of having coronary artery disease
Evaluate the effectiveness of your cardiac treatment plan
Can I eat or drink on the day of the test?
Yes. However, DO NOT eat or drink anything except water for four hours before the test.
Avoid all products that contain caffeine for 24 hours before the test. In general, caffeine is found in coffee, tea, colas and other soft drinks, most chocolate products, as well as strawberries (these contain a small amount of caffeine), as caffeine will interfere with the results of the test. Also avoid decaffeinated or caffeine-free products for 24 hours before the test, as these product contain trace amounts of caffeine.
DO NOT SMOKE ON THE DAY OF THE TEST, as nicotine will interfere with the results of your test.
Should I take my medications the day of the test?
Since many over-the-counter medications contain caffeine (such as diet pills, NoDoz®, Excedrin® and Anacin®), DO NOT take any over-the-counter medication that contains caffeine for 24 hours before the test. Ask your physician, pharmacist or nurse if you have questions about other medications that may contain caffeine.
DO NOT take the following heart medications on the day of your test unless your physician tells you otherwise or if it is needed to treat chest discomfort the day of the test:
Beta blockers (e.g., atenolol (Tenormin), carvedilol (Coreg), metoprolol (Lopressor, Toprol), Propranolol (Inderal))
Isosorbide dinitrate (e.g., Dilatrate®, Isordil®, Sorbitrate®)
Isosorbide mononitrate (e.g., Ismo®, Imdur®, Monoket®)
Nitroglycerin (e.g., Minitran®, Nitropatches®, Nitrostat®)
Your physician may also ask you to stop taking other heart medications on the day of your test. If you have any questions about your medications, ask your physician.
If you use an inhaler for your breathing, please bring it to the test.
NOTE: Do not discontinue any medication without first talking with your physician.